
Left to RightShunts
Left to RightShunts
© William Herring, MD, FACR

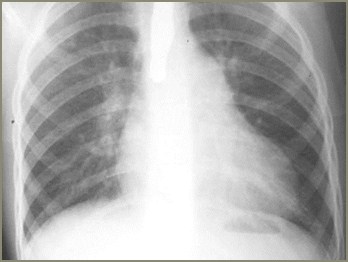
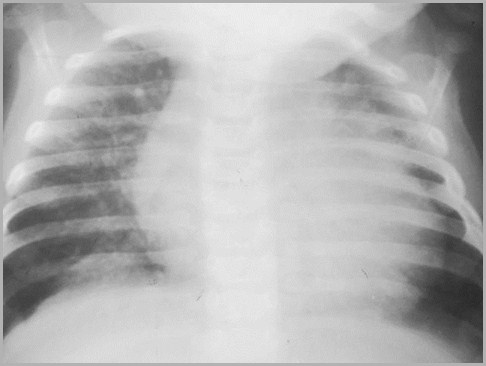
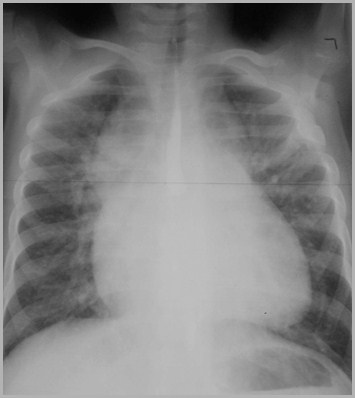
7 yo acyanotic female
What’s the diagnosis?

Atrial Septal Defect

Atrial Septal DefectFour Major Types
Ostium secundum
Ostium primum
Sinus venosus
Posteroinferior

Atrial Septal DefectGeneral
4:1 ratio of females to males
Most frequent congenital heart lesioninitially diagnosed in adult
Frequently associated with Ellis-vanCreveld and Holt-Oram syndromes
Associated with prolapsing mitral valve


Holt-Oram Syndrome –Absence or hypoplasia of the radial ray

Atrial Septal DefectOstium Secundum Type
Most common is ostium secundum(60%) located at fossa ovalis
High association with prolapse ofmitral valve

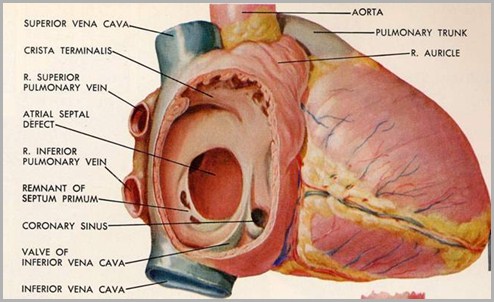
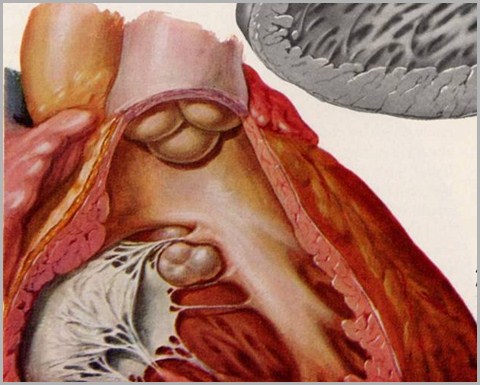
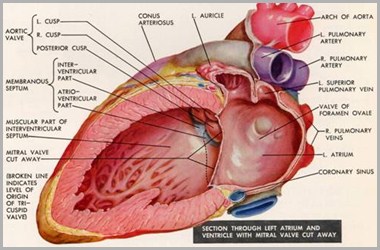
Right atrium open looking into leftatrium through ASD
Normal
© Frank Netter, MD Novartis®

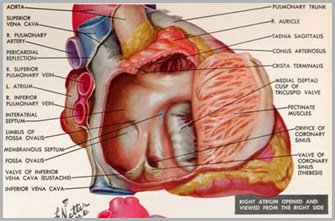
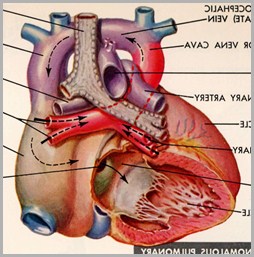
Atrial Septal DefectOstium Primum Type
Ostium primum type usually part ofendocardial cushion defect
Frequently associated with cleftmitral and tricuspid valves
Tends to act like VSD physiologically

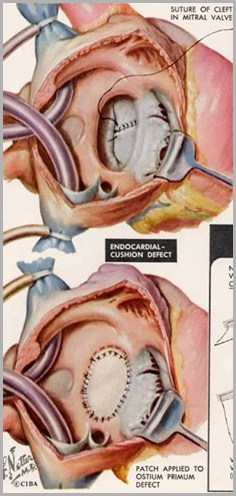
Looking throughostium primum defectat cleft mitral valve
Proximity of ostiumprimum defect totricuspid valve
© Frank Netter, MD Novartis®

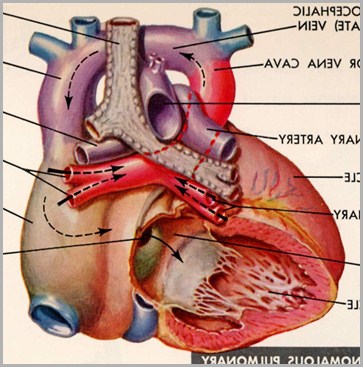
Atrial Septal DefectSinus Venosus Type
Sinus venosus type located high ininter-atrial septum
90% association of anomalous drainageof R upper pulmonary vein with SVCor right atrium
Partial anomalous pulmonary venous return

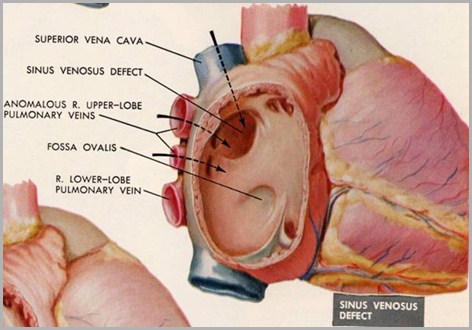
Right atrium open looking into left atrium through ASD
© Frank Netter, MD Novartis®

Atrial Septal DefectPosteroinferior Type
Most rare type
Associated with absence of coronarysinus and left SVC emptying into LA

Atrial Septal DefectPulmonary Hypertension
Rare in ostium secundum variety (<6%)
Low pressure shunt from LA RA
More common in ostium primum variety
Behaves physiologically like VSD

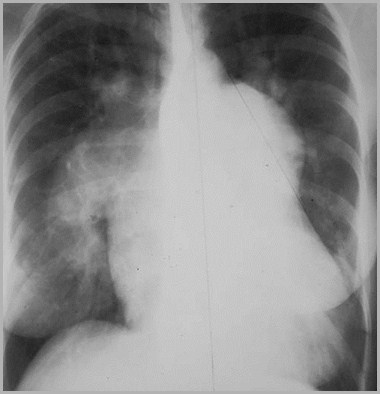
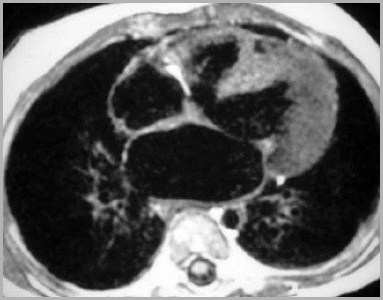
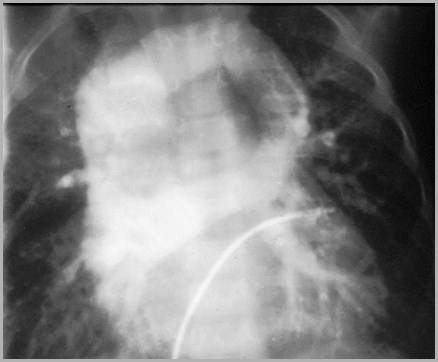
37 yo female with severe PAH 2°ostium primum type of ASD

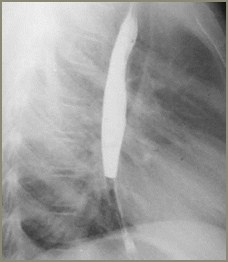
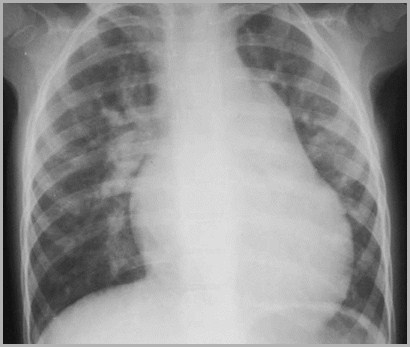
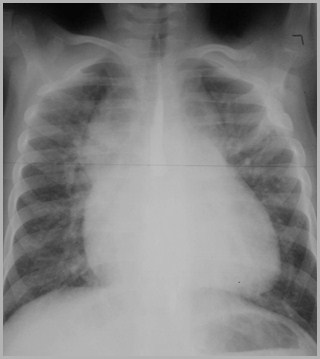
Atrial Septal DefectX-Ray Findings
Enlarged pulmonary vessels
Normal-sized left atrium
Normal to small aorta

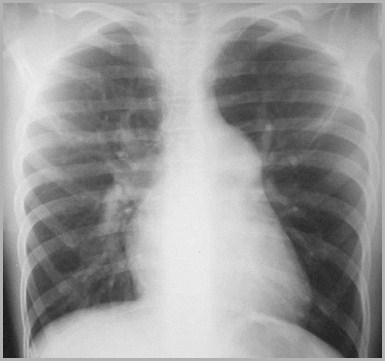
ASD
Prominentpulmonaryvessels
ProminentMPA
Normal leftatrium

Atrial Septal DefectComplications
Large shunts associated with
Pulmonary infections and cardiac arrythmias
Higher incidence of pericardial diseasewith ASD than any other CHD
Bacterial endocarditis is rare

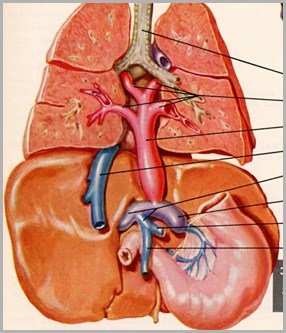
LA
Ao
ASD
PDA
VSD
Differentiating ASD, PDA and VSD

Atrial Septal DefectWhy the Left Atrium Isn’t Enlarged
LA
RA
RV
LV

Ostium SecundumASD
Amersham
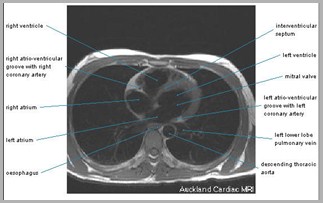
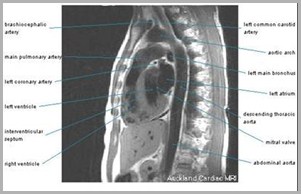
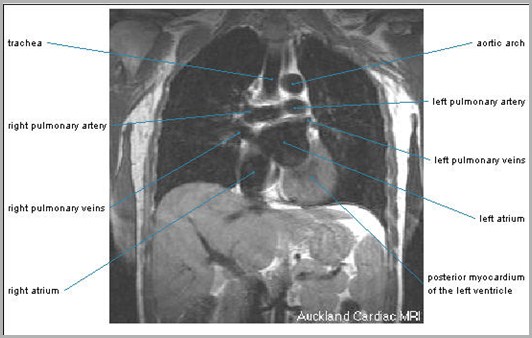
Auckland MRI

• Discontinuity in the atrial septum with systolic signal void consistent with L->R shunton atrial level
• Right atrium is mildly dilated; RV, LV and LA size are normal

SCMR
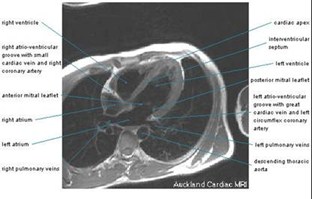

Auckland MRI

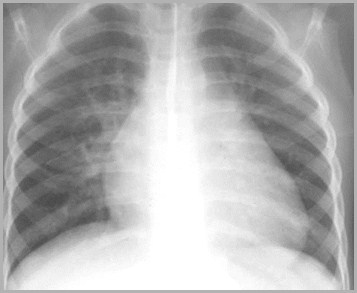
1 yo acyanotic female
What’s the diagnosis?

Ventricular SeptalDefectVentricular SeptalDefect

Ventricular Septal DefectGeneral
Most common L R shunt
Shunt is actually from left ventricle intopulmonary artery more than into rightventricle

Ventricular Septal DefectTypes
Membranous
Supracristal
Muscular
AV canal

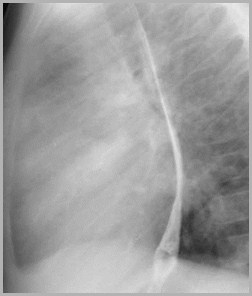
Ventricular Septal DefectMembranous
Membranous = perimembranous VSD(75-80%–most common)
Location: Posterior and inferior tocrista supraventricularis near rightand posterior (=non-coronary) aorticvalve cusps
Associated with: small aneurysms ofmembranous septum

Right ventricle opened
Cristasupraventricularis
Membranous VSD
Normal
© Frank Netter, MD Novartis®

Aneurysm ofmembranousseptum
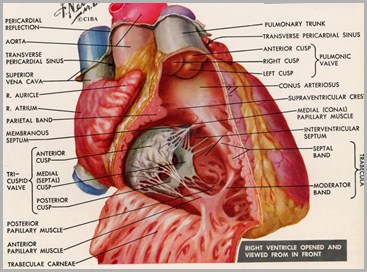
Normal
© Frank Netter, MD Novartis®

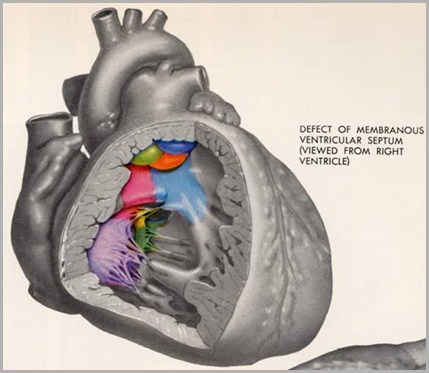
Ventricular Septal DefectSupracristal
Supracristal = conal VSD (5%–leastcommon)
Crista supraventricularis= inverted U-shaped muscular ridge posterior andinferior to the pulmonic valve high ininterventricular septum
Right aortic valve cusp may herniate aortic insufficiency

Ventricular Septal DefectMuscular
Muscular VSD (5–10%)
Low and anterior within trabeculationsof muscular septum
May consist of multiple VSDs = “Swiss-cheese septum”

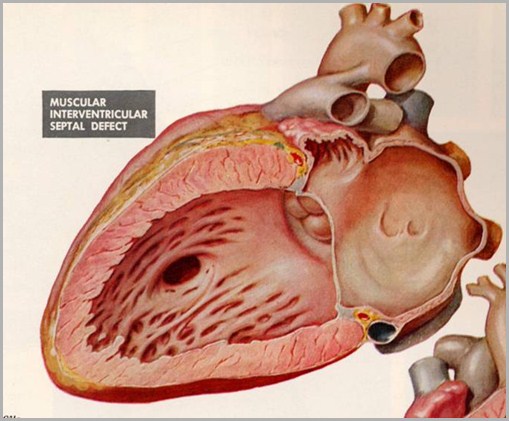

Swisscheese
© Frank Netter, MD Novartis®

Ventricular Septal DefectAV Canal
Atrioventricular canal = endocardialcushion type = posterior VSD (5–10%)
Location: adjacent to septal andanterior leaflet of mitral valve
Large VSD pulmonary hypertension,eventually shunt reversal
Eisenmenger’s physiology
Very large VSD CHF soon after birth

Large posterior VSD(AV canal)
© Frank Netter, MD Novartis®

Ventricular Septal DefectNatural History
Natural history of VSD is affected bytwo factors:
Location of defect
Muscular and perimembranous have highincidence of spontaneous closure
Endocardial cushion defects have low rate ofclosure

Ventricular Septal DefectNatural History
Size of the defect
Larger the defect, more likely to CHF
Smaller the defect, more likely to beasymptomatic

Ventricular Septal DefectEisenmenger Physiology
Progressive increase in pulmonaryvascular resistance
Intimal and medial hyperplasia
Reversal of L R shunt to R L shunt
Cyanosis
Serial chest x-rays may showdecrease in size of pulmonary vessels

Ventricular Septal DefectClinical Course
Neonates usually asymptomaticbecause of high pulmonary vascularresistance from birth to 6 weeks
Common cause of CHF in infancy
Bacterial endocarditis may develop
Severe pulmonary hypertension Eisenmenger’s physiology/cyanosis

Ventricular Septal DefectX-ray Findings
Prominent main pulmonary artery
Adult
Shunt vasculature (increased flow tothe lungs)
LA enlargement (80%)
Aorta normal in size

LA
RA
RV
LV
Ventricular Septal DefectWhy Left Atrium Is Enlarged

VSD

Ventricular Septal DefectPrognosis
Spontaneous closure occurs in40% during first 2 years of life
60% by 5 years

Ventricular Septal DefectIndications For Surgery
Greater than 2:1 shunt, surgery requiredbefore pulmonary arterial hypertensiondevelops
CHF unresponsive to medical management
Failure to grow
Supracristal defects because of theirhigh incidence of AI


Amersham
Membranous VSD
Auckland MRI

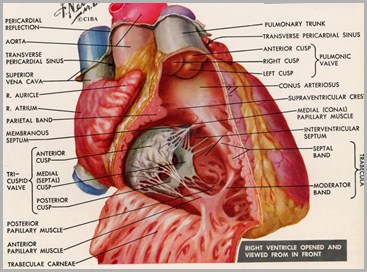
8 mos old acyanotic female

What’s the diagnosis?

Patent DuctusArteriosusPatent DuctusArteriosus

Patent Ductus ArteriosusGeneral
Higher incidence in
Trisomy 21
Trisomy 18
Rubella
Preemies
Predominance in females 4:1

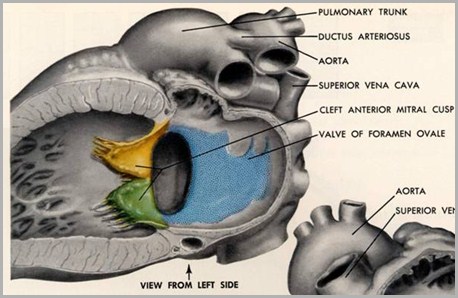
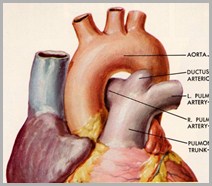
Patent Ductus ArteriosusAnatomy
Ductus connects pulmonary artery todescending aorta just distal to leftsubclavian artery

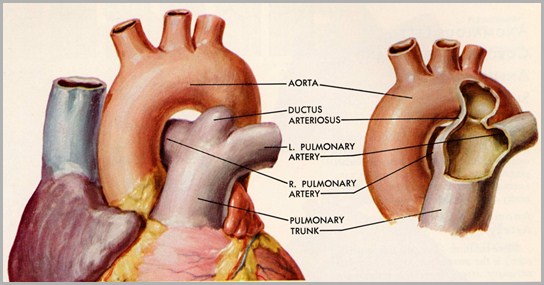
Ductus Arteriosus
© Frank Netter, MD Novartis®

Ductus ArteriosusPhysiology
In fetal life, shunts blood frompulmonary artery to aorta
At birth, increase in arterial oxygenconcentration constriction ofductus

Ductus ArteriosusNormal Closure
Functional closure
By 24 hrs of life
Normal anatomic closure
Complete by 2 months in 90%
Closure at 1 year in 99%

Patent Ductus ArteriosusPathophysiology
Ductus may persist
Because of defect in muscular wall of ductus, or
Chemical defect in response to oxygen
Anatomic persistence of ductusbeyond 4 months is abnormal
Blood is shunted from aorta topulmonary arteries


Patent Ductus ArteriosusClinical
Common cause of CHF in prematureinfants
Usually at age 1 week (after HMD subsides andpulmonary arterial pressure falls)
Wide pulse pressure
Continuous murmur

Patent Ductus ArteriosusX-ray Findings
Cardiomegaly
Enlarged left atrium
Prominent main pulmonary artery (adult)
Prominent peripheral pulmonary vessels
Prominence of ascending aorta

PDA

Patent Ductus ArteriosusWhy Left Atrium Is Enlarged
LA
RA
RV
LV

Patent Ductus ArteriosusCalcifications
Punctate calcification at site of closedductus is normal finding
Linear or railroad track calcification atsite of ductus may be seen in adultswith PDA

Patent Ductus ArteriosusPrognosis
Spontaneous closure may occur

Patent Ductus ArteriosusComplications
CHF
Failure to grow
Pulmonary infections
Bacterial endocarditis
Eisenmenger’s physiology with advancedlesions

• Jet of signal loss showing continuous flow from the aorta to the MPAconsistent with sizeable PDA
• MPA is severely dilated at level of PDA
SCMR

Auckland MRI
Auckland MRI

2 yo old cyanotic female
What’s the diagnosis?

Partial or TotalAnomalous PulmonaryVenous ReturnPartial or TotalAnomalous PulmonaryVenous Return

Cyanosis With IncreasedVascularity
Truncus types I, II, III
TAPVR
Tricuspid atresia*
Transposition*
Single ventricle
* Also appears on DDx of Cyanosis with Inc Vascularity

CHF In NewbornImpede Return of Flow to Left Heart
Infantile coarctation
Congenital aortic stenosis
Hypoplastic left heart syndrome
Congenital mitral stenosis
Cor triatriatum
Obstruction to venous return fromlungs
TAPVR from below diaphragm

Two Types
Partial (PAPVR)
Mild physiologic abnormality
Usually asymptomatic
Total (TAPVR)
Serious physiologic abnormalities

Normal heart
Return ofblood fromlungs is byfour pulmonaryveins to LA
RA
LA
RV
LV
PA
Ao

PAPVRGeneral
One or two of four pulmonary veins maydrain into right atrium
Mild or no physiologic consequence
Associated with ASD
Sinus venosus or ostium secundum types

Partial Anomalous Pulmonary Return
Return ofblood fromlungs is mostlyto LA
One veinabnormallyconnected toright heart
Frequentlyassociated withsinus venosusor secundumASD
RA
LA
RV
LV
PA
Ao


PAPVR
Auckland MRI
Korean Journal of Radiology

TAPVRGeneral
All have shunt through lungs R heart
All must also have R L shunt forsurvival
Obligatory ASD to return blood to the systemicside
All are cyanotic
Identical oxygenation in all four chambers

TAPVRTypes
Supracardiac
Cardiac
Infracardiac
Mixed

TAPVRSupracardiac Type—Type I
Most common (52%)
Pulmonary veins drain into verticalvein (behind left pulmonary artery)left brachiocephalic vein SVC
DDx: VSD with large thymus

Leftsuperiorvena cava
Rightsuperiorvenacava
Left Brachiocephalic vein
Verticalvein
TAPVR-Supracardiac Type 1
Pulmonaryveins
Rightatrium
© Frank Netter, MD Novartis®

TAPVR-SupracardiacType 1
© Frank Netter, MD Novartis®

TAPVRSupracardiac Type 1—X-ray Findings
Snowman heart = dilated SVC+ leftvertical vein
Shunt vasculature 2° increased returnto right heart
Enlargement of right heart 2° volumeoverload

TAPVR-Supracardiac Type 1

RA
LA
RV
LV
PA
Ao
TAPVR–Type I–Supracardiac type
Blood movesthrough Lbrachiocephalic vto R SVC
Blood fromlungs drainsinto left verticalveinto L SVC
Increasedreturn to rightheart overloadslungs shunt vessels
ASD provides R L shunt toallowoxygenatedblood to reachbody (moderatecyanosis)

TAPVRCardiac Type—Type II
Second most common: 30%
Blood from lungs coronary sinus or RA
Coronary sinus more common
Overload of RV CHF after birth
Increased pulmonary vasculature
20% of I’s and II’s survive to adulthood
Remainder expire in first year

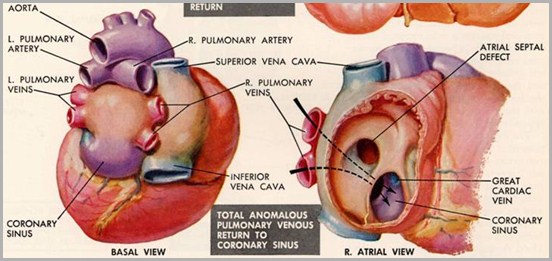
TAPVR-Coronary Sinus-Type II
Coronarysinus
© Frank Netter, MD Novartis®

TAPVR
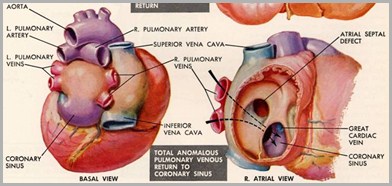
© Frank Netter, MD Novartis®
Pulmonary veins

TAPVR–Type II–Cardiac Type
Blood returnsfrom lung to RAor coronary sinus
ASD provides R L shunt toallowoxygenatedblood to reachbody (moderatecyanosis)
Increasedreturn to rightheartoverloadslungs shunt vessels
RA
LA
RV
LV
PA
Ao

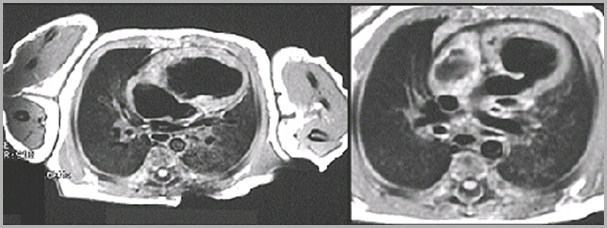
TAPVRInfracardiac Type—Type III
Percent of total: 12%
Long pulmonary veins course downalong esophagus
Empty into portal vein (morecommon) or IVC
Vein constricted by diaphragm as itpasses through esophageal hiatus

TAPVR-Type III-Infradiaphragmatic
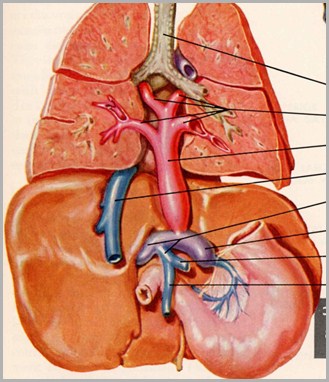
Portal vein
Pulmonaryveins
© Frank Netter, MD Novartis®

TAPVRInfracardiac Type—Continued
Severe CHF (90%) 2° obstruction tovenous return
Cyanotic 2° right left shuntthrough ASD
Associated with asplenia (80%), orpolysplenia
Prognosis=death within a few days

TAPVR–Type III–Infracardiac type
ASD providesR L shunt toallowoxygenatedblood to reachbody (cyanotic)
CHF vasculature
RA
LA
RV
LV
PA
Ao
Blood returningfrom lungs pulmonary veinswhich areconstricted bydiaphragm CHF
To portal v IVC RA

TAPVRMixed Type—Type IV
Percent of total: 6%
Mixtures of types I – III


TAPVR
© Frank Netter, MD Novartis®
University of Minnesota

The End